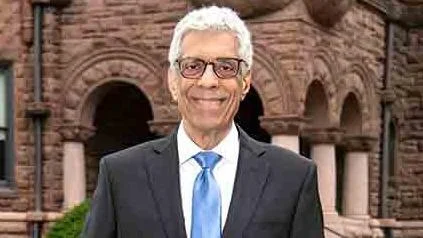
Dr. Fred Pestello, President | St. Louis University
Dr. Fred Pestello, President | St. Louis University
Patients with post-traumatic stress disorder (PTSD) and type 2 diabetes face more severe health challenges than those with diabetes alone, according to a study by Saint Louis University. The research highlights that PTSD can negatively impact glycemic control, increase hospitalization risks, and worsen self-reported health outcomes.
Jeffrey Scherrer, Ph.D., a professor at Saint Louis University School of Medicine and the senior author of the study, stated, "To our knowledge, this is the first evidence that PTSD is a modifiable risk factor, albeit a modest one, for some adverse diabetes outcomes such as microvascular complications."
Scherrer emphasized the importance of addressing both mental and physical health in patients with comorbid PTSD and diabetes. He said, "This is further evidence that we should not separate mental from physical health. Treating the whole patient with comorbid PTSD and diabetes should address both conditions to optimize outcomes. Screening for and treating PTSD as part of diabetes care may lead to better clinical outcomes for both conditions."
The study analyzed data from 10,002 Veterans Health Administration (VHA) patients aged 18 to 80 with both PTSD and type 2 diabetes over an eleven-year period from 2011 to 2022. Results indicated that improvements in PTSD symptoms correlated with an 8% reduction in risk for microvascular complications among these patients.
Furthermore, younger patients aged 18-49 who no longer met the criteria for PTSD showed a significantly lower risk of insulin initiation and all-cause mortality compared to those still diagnosed with PTSD.
The study suggests that physiological abnormalities linked to metabolic hormones and inflammatory responses could explain the relationship between PTSD and type 2 diabetes. The authors include experts from various institutions such as Washington University School of Medicine, Geisel School of Medicine at Dartmouth, University of California San Francisco School of Medicine, Mayo Clinic, among others.
This research received funding through grant R01HL160553 from the National Heart, Lung, and Blood Institute.


 Alerts Sign-up
Alerts Sign-up